Are you a journalist? Please sign up here for our press releases
Subscribe to our monthly newsletter:
A team of researchers led by Prof. Irun Cohen of the Weizmann Institute of Science has developed a vaccine that halts the progression of Type I (juvenile or insulin-dependent) diabetes. The vaccine functions by blocking the destruction of insulin-secreting pancreatic cells.
Diabetes is a chronic disease associated with elevated blood sugar levels, in which the body does not produce or improperly uses insulin - a hormone needed to convert sugar, starches and other foods into energy. Recent data show that between 120 and 140 million people suffer from diabetes worldwide. Type I diabetes usually results from an autoimmune disorder in which the immune system mistakenly attacks the body's own insulin-producing pancreatic cells, reducing and ultimately eliminating all insulin production. All Type I diabetes patients eventually must receive insulin injections to compensate for their loss of natural insulin production.
For the past several years researchers at the Weizmann Institute's Department of Immunology led by Cohen have been studying the mechanism by which the immune system destroys the insulin-producing pancreatic cells. Working with mice, the scientists discovered that a particular protein called HSP60 was closely linked to this destructive process.
The protein acts like an antigen, prompting the immune cells to attack. Further investigation by Cohen, Dr. Dana Elias (first a graduate student and then a postdoctoral fellow at the Institute), and other students and colleagues revealed that injecting sick mice with p277, a small peptide fragment of the HSP60 protein, shut down the immune response, preventing the progression of Type I diabetes. This led Peptor Ltd., a biopharmaceutical company based in Rehovot, Israel, to develop the experimental drug DiaPep277, designed to prevent or treat Type I diabetes.
A combined clinical study performed recently by researchers at Hadassah-Hebrew University Medical School, Peptor Ltd., and Cohen proved that DiaPep277 is successful in arresting the progression of Type I diabetes in newly diagnosed patients. The research findings were published in the Lancet.
The study involved 35 patients newly diagnosed with Type I diabetes. Eighteen patients received injections of DiaPep277 - at the beginning of the study, after one month, and after six months; 17 patients received three injections of an inert substance (a placebo). Patients in the treatment group (those receiving DiaPep277) showed a delay or even a cessation in the attack by the immune system upon their pancreatic insulin-producing cells. These results were evident in the level of the body's own insulin production and a decreased need for insulin injections. The researchers were able to trace the mechanism of this improvement to changes in the patients' immune lymphocytes called T-cells. In contrast, patients receiving the placebo showed a significant decline in their natural insulin production and a persistent rise in the need for insulin injections. No significant side effects as a result of injecting DiaPep277 were found.
'The idea of using p277 stemmed from the discovery that the immune system has different options to choose from in responding to an antigen,' says Cohen. 'It can act to destroy the antigen or alternatively protect it from being destroyed. In the latter case it protects the antigen, thereby indirectly preventing damage to the pancreatic cells. The peptide essentially acts to 'reeducate' the immune cells, switching off their destructive activity.'
The scientists participating in this study are: Prof. Itamar Raz and Dr. Muriel Metzger of Hadassah-Hebrew University Medical School; Dr. Dana Elias (now VP R&D at Peptor Ltd.); and Drs. Ann Avron and Merana Tamir, also of Peptor Ltd.
Back in 1920 Dr. Federick Banting and Charles Best of the University of Toronto made a discovery that would change the course of medical history. They had succeeded in obtaining a pancreatic extract which proved to have potent anti-diabetic characteristics when tested on dogs. Within two years their team would isolate and purify the extract's key ingredient, a hormone known as insulin, and the first human trial would begin, extending the life of Leonard Thomson, a fourteen year-old-boy who lay dying in hospital, for an additional 13 years.
Today extensive research efforts have yielded dramatically improved high-quality insulin as well as better delivery methods. Nevertheless insulin is not a cure, it merely helps to maintain blood sugar levels in check. A cure would be to stop the autoimmune destruction, sparing the insulin-producing beta cells. In contrast to the replacement therapy offered by insulin, the vaccine currently in development by Prof. Cohen's team has been shown to prevent the destruction of pancreatic cells.
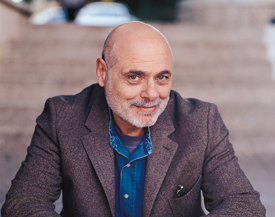
Prof. Cohen holds the Helen and Morris Mauerberger Professorial Chair in Immunology. His research is supported by the Robert Koch Minerva Center for Research in Autoimmune Disease, the Yeshaya Horowitz Association, and Mr. and Mrs. Samuel T. Cohen, Illinois.