Are you a journalist? Please sign up here for our press releases
Subscribe to our monthly newsletter:
Cell death – or cells’ refusal to die – is the subject of a great deal of research and a topic that has crucial implications for our health. As reported recently in Nature Communications, Weizmann Institute researchers have now discovered an entirely new mechanism of cell death – a discovery that may have wide-ranging implications for understanding and treating disease.
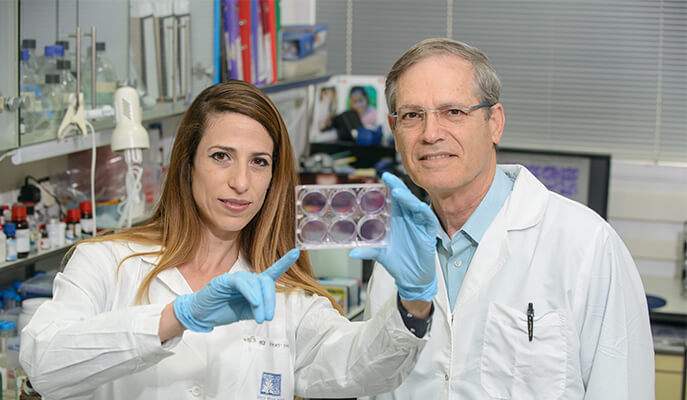
The team of Prof. Menachem Rubinstein of the Molecular Genetics Department – graduate student Efrat Dvash, who led the study, Michal Har-Tal, Ofir Meir, and Sara Barak – showed that cells may die as a result of a previously unknown chain of events. It starts with the Mgst2 gene, which becomes activated when the cell is under stress. This leads to the creation of a small fatty molecule called leukotriene C4, which triggers the production of reactive oxygen molecules that damage DNA, ultimately killing the cell.
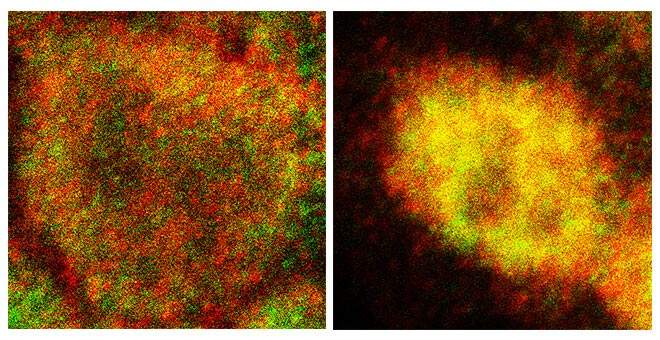
In a series of experiments, the scientists confirmed that Mgst2 indeed acts as a switch for this type of cell death and that leukotriene C4 is a major player in executing the death command. The researchers created mice that lack the Mgst2 gene and found that these mice were much more resistant to toxic agents that normally prompt cell death.
Administering asthma drugs to block leukotriene could prevent the death of healthy cells throughout the patient’s body
Leukotrienes have long been known to be produced by the mast cells of the immune system; they are implicated in triggering the symptoms of asthma and allergy. In fact common asthma drugs, known by the generic names montelukast and pranlukast, work by blocking leukotriene action. The Weizmann study revealed that upon exposure to stress-causing toxic agents, virtually all body cell types can produce leukotriene C4, and that this small molecule can, on its own, trigger DNA damage and cell death.
Because cell death is so central to numerous aspects of human health and disease, the discovery of an entirely new mechanism for its control applies to a host of normal and pathological situations. It may, for example, enable safer chemotherapy for blood malignancies, help clarify the mechanism underlying Alzheimer’s disease and other neurodegenerative disorders, and lead to improved methods of stimulating the healing of fractured bones.
The most immediate application may be for cancers of the blood: Although many chemotherapy drugs kill malignant cells by activating Mgst2 and leukotriene C4, they apparently work with a different means of cell death to destroy blood cancer cells. Administering asthma drugs to block leukotriene could therefore prevent the death of healthy cells throughout the patient’s body and thus reduce some of the toxic side-effects.
An additional direction of research instigated by the Weizmann study concerns the muscle pain felt by a significant portion of patients who take statins. These widely-prescribed cholesterol-lowering drugs are thought to cause pain by triggering muscle cell death. Rubinstein’s team is currently investigating the involvement of Mgst2 and leukotriene C4 in the death of muscle cells in laboratory animals.
The prescription asthma drugs have also been observed to slow the progression of Alzheimer’s disease in mice, and Rubinstein’s group, together with other Weizmann Institute research groups, had shown the involvement of Mgst2 in regulating bone repair. Rubinstein and his group are hopeful that because these drugs have already been shown to be safe for humans, they will enter clinical trials for these various diseases and side-effects in the near future.
Prof. Menachem Rubinstein's research is supported by the Jeanne and Joseph Nissim Foundation for Life Sciences Research; the Bernard and Audrey Jaffe Foundation; and the Florence Blau Charitable Trust. Prof. Rubinstein is the incumbent of the Maurice and Edna Weiss Professorial Chair of Cytokines Research.