Are you a journalist? Please sign up here for our press releases
Subscribe to our monthly newsletter:
Our blood is constantly replenished by new arrivals minted from a small pool of dedicated stem cells in the bone marrow. Throughout this process, a secure cache of blood stem cells is always left behind: They divide without losing their stem-cell properties, so that the life-sustaining source of blood in the bone marrow never dries up. It is these stem cells that are extracted from donors when people with cancers like leukemia require bone marrow transplants. But when the supply of blood stem cells for transplantation is limited, there's no way of increasing it because scientists still can't grow these cells in the laboratory without causing them to lose their vital capacity for self-renewal.
New research at the Weizmann Institute of Science may help produce blood stem cells in larger numbers – a finding that can facilitate bone marrow transplantation in many cases. For instance, when people in need of a transplant lack a perfectly matched donor, megadoses of stem cells may help overcome the mismatch. When the source of the transplant is blood from the umbilical cord, which contains only few stem cells, increasing their numbers can also be crucial for the success of the procedure.

Prof. Idit Shachar of the Immunology Department and her team studied the functions of a receptor known as CD74 – a protein expressed in the membranes of certain blood cells that binds to an immune-regulating molecule referred to as MIF. In previous research, they had learned that this receptor improves the survival of white blood cells called B lymphocytes. In the current study, they wanted to find out if it performs a similar function in the membranes of blood stem cells.
Surprisingly, it turned out that CD74's function in stem cells is just the opposite: It can trigger a chain of biochemical reactions causing these cells to die. The receptor can probably perform such opposing functions in the two cell types because of the striking differences in oxygen levels and other conditions prevailing in the cellular environment – bloodstream in the case of B lymphocytes, and bone marrow in the case of blood stem cells. When the researchers created genetically engineered mice that lacked CD74, the numbers of blood stem cells in the mouse bone marrow soared. In other words, eliminating the receptor prevented the death of these cells, causing them to survive longer and, consequently, to accumulate in larger numbers.
Shachar: ""Our research may help produce stem cells for transplantation in larger numbers and of a higher quality""
Not only that, but the CD74-lacking stem cells were much better than regular stem cells at transplanting themselves into mice lacking a bone marrow. When the scientists transplanted into such mice a graft consisting of two types of stem cells in equal numbers – with and without CD74 – the ones lacking the CD74 engrafted themselves with much greater success, multiplied and soon took over the entire bone marrow.
The scientists then performed a series of "competition" experiments in which they gradually skewed the ratio, implanting each time relatively more stem cells with CD74 than without. Even so, the CD74-lacking stem cells were much more successful at engraftment, taking over much of the bone marrow even when they made up only about one-tenth of the transplant. In other experiments, mice lacking CD74 stem cells also proved better than the controls at surviving and recovering their immune systems after chemotherapy.
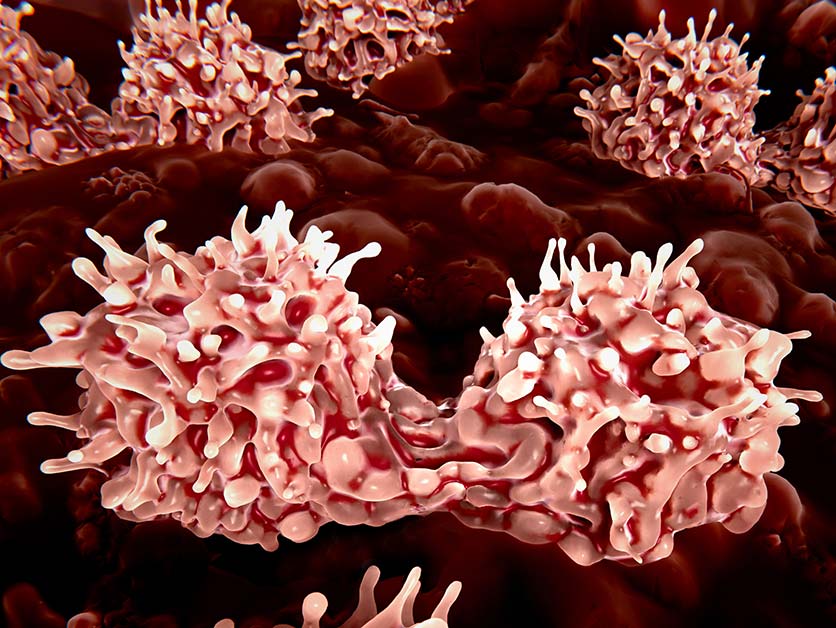
Finally, the researchers showed that CD74 blocking can indeed be developed into a method relevant to human stem cell transplants. By applying an antibody that blocks the active site of CD74, they caused larger numbers of blood stem cells to accumulate both in a laboratory dish and in the bone marrow of mice. In addition, blocking CD74 on human blood stem cells resulted in molecular changes that were similar to those observed in mice.
"Our research may help produce stem cells for transplantation in larger numbers and of a higher quality," Shachar says.
The research team included Dr. Shirly Becker-Herman, Milena Rozenberg, Dr. Carmit Hillel-Karniel, Dr. Naama Gil-Yarom, Dr. Mattias Kramer, Dr. Avital Barak, Dr. Lital Sever, Keren David, Dr. Lihi Radomir, Hadas Lewinsky and Michal Levi of Weizmann's Immunology Department; Dr. Gilgi Friedlander of the Nancy and Stephen Grand Israel National Center for Personalized Medicine; Prof. Richard Bucala of Yale School of Medicine; and Prof. Amnon Peled of Hadassah Medical Center.
More than 50,000 bone marrow transplants are performed annually around the world – and this figure is constantly on the rise.
Prof. Idit Shachar is the incumbent of the Dr. Morton & Anne Kleiman Professorial Chair.
Prof. Shachar's research is supported by the Benoziyo Endowment Fund for the Advancement of Science; the Moross Integrated Cancer Center; and the Judy and Bernard Briskin Multiple Myeloma Research Project.