Autoimmune diseases can be likened to a sweeping forest fire in which the immune system attacks one of the body's proteins, mistaking it for an "enemy," and then proceeds to attack other proteins in the affected organ. This relatively recent insight into the "forest fire-like" development and progression of autoimmune diseases demonstrates the daunting challenge faced by researchers seeking to block their advance.
Why autoimmune diseases occur is still a mystery, but they appear to stem from the immune system's failure to distinguish between foreign, disease-causing agents and the body's own proteins. Juvenile diabetes, for instance, is caused when a protein essential for the proper functioning of insulin-producing cells is mistakenly attacked, while multiple sclerosis develops when the immune system erroneously attacks the myelin sheath around nerve fibers in the central nervous system.
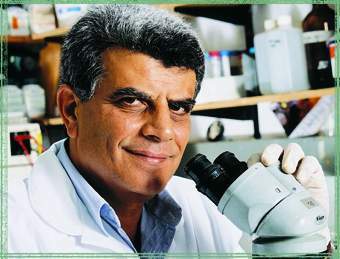
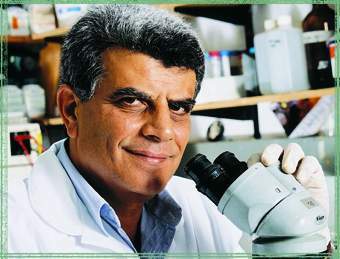
One approach in the struggle against autoimmune diseases has been to weaken the entire immune system. However, this leaves the body extremely vulnerable, which is why scientists are anxious to find means to selectively target the immune system's faulty attacks against the body's proteins without affecting its ability to combat foreign invaders. To this end, Prof. Avraham Ben-Nun of the Weizmann Institute's Immunology Department has developed a new strategy for treating autoimmune diseases, particularly multiple sclerosis.
For years, scientists studying multiple sclerosis assumed that the immune system's attack on myelin focused on one of myelin's most abundant proteins, called myelin basic protein, or MBP. Further studies, showed, however, that the attack can also be directed against another myelin protein, called proteolipid protein, or PLP. And the list continued to grow. Several years ago, Ben-Nun and Dr. Nicole Kerlero de Rosbo showed that a third protein, myelin oligodendrocyte glycoprotein, or MOG, is also targeted; and recently Ben-Nun and his colleagues discovered two additional myelin proteins that draw the immune system's "fire" in multiple sclerosis.
These findings drove home the complexity of uncovering autoimmune disease processes. Further studies revealed that not only can a mistaken immune attack against any of these five proteins trigger multiple sclerosis, but the major proteins targeted can vary from patient to patient, and in a given patient at different stages of the disease. Just like a forest fire, the immune attack may initially target one protein but then spread to any or several of the other five proteins, sequentially or simultaneously, while often abandoning the original target.
It became clear that to selectively suppress harmful autoimmune responses without shutting down the entire immune system one would have to identify the specific proteins targeted in each patient at any given stage - a process requiring complex, expensive, and time-consuming tests. Ben-Nun set out to devise a therapy theoretically suitable for most patients - one that would selectively neutralize an autoimmune attack against any of the five proteins, regardless of which protein is attacked. For this purpose his team identified the main "draw-fire" regions on each of the five target proteins, using biological testing methods and computer modeling in collaboration with Dr. Miriam Eisenstein of the Weizmann Institute's Chemical Services Unit. Then, using genetic engineering, Ben-Nun with the assistance of Dr. Lydia Cohen, generated a synthetic gene in which all of these regions are encoded in a sequential molecular chain. This synthetic gene was subsequently introduced into bacteria, which then produced the novel "draw-fire regions" protein - a protein that does not exist in nature.
When administered under certain conditions, this genetically engineered protein was found to protect mice against multiple sclerosis-like disease whereas injection under other conditions led to disease onset. Ben-Nun and his colleagues also demonstrated that it is possible to vaccinate mice against the disease using the gene itself. When incorporated into mouse cells, this gene serves as a "data bank," allowing the cells to manufacture the "draw-fire regions" protein, thus eliminating the need for continuous protein administration. This strategy was employed by the Institute scientists to design synthetic genes coding for "draw-fire regions" proteins pertinent to immune-specific therapies for several autoimmune diseases: a protein called Y-MSP for potential treatment of multiple sclerosis, Y-DMP for juvenile diabetes, and Y-RAP for rheumatoid arthritis. Yeda Research & Development Co. has filed a patent application for this approach.
In current studies Ben-Nun and his colleagues are further developing their approach to produce genetically engineered "draw-fire regions" proteins modified to effectively suppress these autoimmune diseases without triggering other disease processes.
Other scientists participating in this study were Dr. Gregor Sappler and research students Itzhack Mendel, Ming-Chao Zhong, and Joel Kay, all of the Weizmann Institute's Immunology Department; Dr. Roni Milo, Neurology, Assaf Harofeh Medical Center; Prof. Oded Abramsky, Neurology, Hadassah University Hospital; and Dr. Michael Hoffman and Prof. Israel Yust, Internal Medicine, Ichilov Medical Center.