The white blood cells that fight disease and help our bodies heal are directed to sites of infection or injury by “exit signs” – chemical signals that tell them where to pass through the blood vessel walls and into the underlying tissue.
New research at the Weizmann Institute, which appeared in
Nature Immunology online, shows how the cells lining blood vessel walls may act as “selectors” by hiding the signals where only certain “educated” white blood cells will find them.
In previous studies,
Prof. Ronen Alon and his team in the Immunology Department had found that near sites of inflammation,
white blood cells rapidly crawl along the inner lining of the blood vessels with tens of tiny legs that grip the surface tightly, feeling for the exit sign. Such signs consist of migration-promoting molecules called chemokines, which the cells lining the blood vessels – endothelial cells – display on their outer surfaces like flashing lights.
In the new study, Alon and his team, including Drs. Ziv Shulman and Shmuel Cohen, found that not all chemokine signals produced by endothelial cells are on display. They observed the recruitment of subsets of immune cells called effector cells that are the “special forces” of the immune system: They receive training in the lymph nodes, where they learn to identify a particular newly-invading pathogen and then return to the bloodstream on a search and destroy mission. Like the other white blood cells, effector cells crawled on tiny appendages along the lining of inflamed blood vessels near the site of pathogen entry, but rather than sensing surface chemokines, they used their legs to reach into the endothelial cells in search of the migration-promoting chemokines.
As opposed to the external exit signs, these chemokines were held in tiny containers – vesicles – inside the inflamed endothelial cell walls. The effector cells paused in the joins where several cells met, inserting their legs through the walls of several endothelial cells at once to trap chemokines as they were released from vesicles at the endothelial cell membrane. Once they obtained the right chemokine directives, the immune cells were quickly ushered out through the blood vessel walls toward their final destination.
The researchers think that keeping the chemokines inside the endothelial cells ensures, on the one hand, that these vital signals will be safe from getting washed away in the blood or eaten by various enzymes. On the other hand, it guarantees that only those effector cells with special training – that can make the extra effort to find the signals – will pass through.
Alon: “We are now seeing that the blood vessel endothelium is much more than just a passive, sticky barrier – it actively selects which recruited cells actually cross the barrier and which will not. The endothelial cells seem to play an active role in showing the immune cells the right way out, though we’re not sure exactly how. Moreover, we think that tumors near blood vessels might exploit these trafficking rules for their benefit by putting the endothelial cells in a quiescent state or making the endothelium produce the “wrong” chemokines. Thus, immune cells capable of destroying these tumors will not be able to exit the blood and navigate to the tumor site, while other immune cells that aid in cancer growth will.”
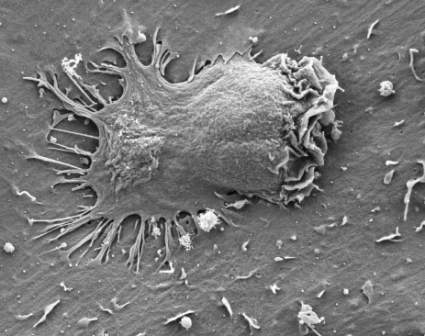
Effector cells, tagged green, seem to fade as they detect chemokines and move inward, past the surface of the blood vessel endothelium
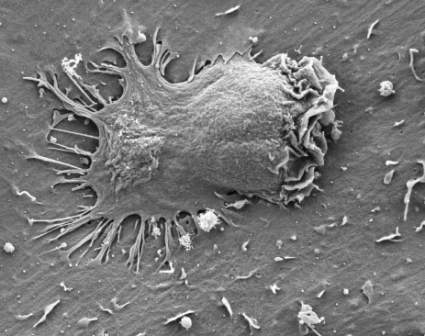
Effector cells in an experimental control move on endothelium that does not produce internal chemokines
Prof. Ronen Alon’s research is supported by the Kirk Center for Childhood Cancer and Immunological Disorders. Prof. Alon is the incumbent of the Linda Jacobs Professorial Chair in Immune and Stem Cell Research.