Prof. Michel Revel was just a teenager when Alick Isaacs and Jean Lindenmann discovered why infection with one virus could prevent disease when a second virus attacked soon after. Until then it was believed that the first virus somehow managed to stymie the second, but the two scientists showed that the cells (in this case in chicken embryos) produce a substance in reaction to viral invasion that has a long-lasting effect. They called this substance interferon, because it interferes with viral activity.
Fifty years later, interferon-based drugs are a multi-billion dollar industry, used for treatment of viral diseases such as hepatitis, some cancers, and multiple sclerosis. Research continues both in new medical applications and in elucidating the ways that this family of molecules works in the body. The Weizmann Institute of Science has played a prominent role in the interferon story.
Prof. Revel arrived at the Weizmann Institute in 1968, with his wife Claire and four young children, after having worked at the Pasteur Institute in Paris on factors that control initiation of protein synthesis. At the Weizmann Institute, he was interested in working on a related subject – one that might have therapeutic applications. Although interferon had been discovered over a decade earlier, almost nothing was known about it. It was difficult to produce, and no one had succeeded in purifying it or producing it in large quantities. Revel met up with a pair of Argentinean scientists doing interferon research in Paris, Ernesto and Rebecca Falcoff, and began to collaborate with them in 1970. Soon, they were publishing an important paper in Nature showing that, for such viruses as the polio virus, which carry their genetic information in the form of RNA (rather than DNA), interferon steps in and controls protein synthesis at the stage in which the instructions carried in the viral RNA are translated into the long strings of amino acids that make up the viral proteins. Prof. Adi Kimchi, then a postdoctoral fellow with Revel, isolated factors explaining how interferon controls the translation stage of protein synthesis.
Other discoveries followed. Dr. Judith Chebath, who is still a member of Revel’s group in the Molecular Genetics Department, identified a group of genes that increase their activity when exposed to interferon, and showed they code for enzymes involved in interferon's anti-viral actions in cells. In 1975, while a visiting scientist at Yale, Revel discovered that interferon communicates with cells via a receptor on the cell wall, and identified the gene for the receptor. By this point, the Weizmann Institute team was already known in the global scientific community as one of three world leaders in research on interferon's mechanisms of action.
By the end of the seventies, the group had decided to work on the type of interferon known as interferon beta. Though other groups in the world were working on interferon alpha, which is made in white blood cells, Revel felt that the beta form, made in most of the body’s cells, might have a special role. Around this time, a prominent interferon researcher pointed out that interferon beta does not show up in blood when it’s injected, and thus predicted scientists would never be able to develop it as a drug.
Fortunately, Amichai Schattner, an MD who had joined Revel’s group for a six-month research stint while completing his specialization, attacked the problem from a new angle. He stayed on for two years, and he and Revel published a paper showing that injected interferon beta leaves tell-tale evidence of its actions in the genes it activates. Not only was the interferon beta research saved, but the field was left wide open for Weizmann Institute researchers to study.
To get a large enough supply of the interferon the team decided to use readily available young human tissue – foreskins from circumcised babies. At first the Jewish ritual circumcisers refused to let the scientists have the foreskins, which are normally buried, but a member of the group, Dr Dalia Gurari, happened to be the niece of the leader of a large Hassidic sect – the Lubavitcher Rebbe – and soon the lab had a steady supply to work with. Foreskin cell cultures turned out to be instrumental in the search for the Interferon beta gene.
Around this time, the race was on to purify interferon. As it is a potent substance, it is produced in extremely tiny amounts, making it quite difficult to isolate. In the mid seventies, Prof. Menachem Rubinstein had received his Ph.D. from the Feinberg Graduate School and gone on to postdoctoral research at the Roche Institute of Molecular Biology in New Jersey. There, he was given the task of purifying interferon – a substance so many others had failed to isolate in the 20 years since its discovery, it had been dubbed “misinterpreton.”
Rubinstein worked day and night on the job using techniques he had developed with his mentor Sid Udenfriend at Roche, and he recruited his wife, Sara, to work as a lab technician while they split the childcare of their two young children. He recalls that a part of the solution to isolating interferon came to him in a dream: When he went to the lab the next day, he found that his dream, indeed, had contained the insight he needed to make the necessary breakthrough. All in all, Rubinstein managed to purify interferon in a record 10 months. According to his contract with Roche, he and his co-researcher Sid Pestka were paid one dollar for the patent for the process. (That patent has since earned the pharmaceutical company billions of dollars.)
Although he had received a number of offers for positions in the US, Rubinstein wanted to return the Weizmann Institute, where he had a position waiting for him in the Organic Chemistry Department. Eventually, he accepted Revel’s invitation to join the Institute’s Virology Department in 1979. Revel was convinced that interferon beta had potential medical uses, and his team had made important progress on a method of producing it. “I was excited, and I managed to get Aharon Meytahl, then director of Yeda, excited about the possibilities,” Revel says. Yeda, the business arm of the Weizmann Institute, set about looking for companies to invest in interferon beta production; eventually, the Swiss pharmaceutical company Serono agreed to Revel’s condition that the manufacturing plant be built in Israel. A fruitful partnership began to develop with the founding of Interpharm, which first produced the foreskin-derived interferon-beta under the name Frone©.
Around this time, Prof. David Wallach of the Biological Chemistry Department, whose main work concerns other, related biological molecules, made an important contribution to interferon research – showing, together with Revel, that the third type of interferon, known as interferon gamma, has a different effect on the immune system than the alpha and beta interferons. In fact, interferon beta is antagonistic to the effects of interferon gamma and, as they later found, this reduces the autoimmune process in multiple sclerosis.
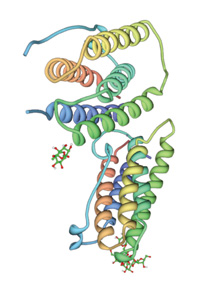
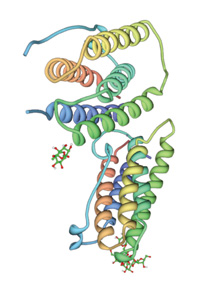
In 1980, having isolated the human gene encoding interferon beta, Revel's group searched for an efficient method to produce the substance in quantity. This brought about another breakthrough. At that time, complex proteins for drugs were produced in bioengineered bacteria or yeast. But these microorganisms don’t know how to add on certain sugar complexes, which seem to act as signals to the immune system identifying the proteins as “self” rather than foreign invaders. To obtain a more useful product, Revel and his team developed a method of producing interferon beta in Chinese hamster ovary cells. They genetically engineered the animal cells to contain 100 copies of the interferon beta gene apiece, and these efficiently generated interferon beta with sugar complexes similar to those in humans. This method has since become a mainstay of the biotech industry.
Revel’s team now began to pursue medical applications for interferon beta, and here another piece of luck came their way. A researcher in the US, who thought a virus might be the cause of multiple sclerosis, was experimenting with treating MS patients with the anti-viral interferon beta. The Weizmann team’s research had shown, however, that interferon also regulates the immune system, and thus can influence immune activities even if no virus is present. They realized the virus theory was wrong, but that interferon beta might prevent the symptoms of MS, in which immune cells mistakenly attack the protective myelin sheaths of nerve cells. Revel convinced Serono to begin conducting trials to develop the treatment.
While work continued on moving interferon beta from the laboratory to the pharmacy, research on the biological properties of this protein continued in the Weizmann Institute labs. Dr. Daniela Novick joined Prof. Revel’s group in the 1979 after receiving her Ph.D. from the Feinberg Graduate School. Together with Prof. Zelig Eshhar of the Immunology Department, she, Rubinstein and Revel developed a relatively simple method for purifying interferon beta, as well as accurate tests for measuring interferon content and purity. They created monoclonal antibodies for interferon and attached them to special polymer beads. When a fluid was passed through a column of these beads, the antibodies pulled interferon molecules out of solution.
At the end of the eighties and heading into the nineties, Weizmann Institute scientists continued to gain important insights into how interferon acts in the body. Rubinstein and Novick, together with Dr. Batya Cohen, had identified a number of cell receptors for various molecules and they applied the techniques they had developed to the purification of interferon, as well. They cloned the receptor that is common to both interferon alpha and beta and characterized it, showing how interferon activates a specific cascade of events within a cell, leading to the immune response.
Rebif©, the interferon beta-based treatment for MS, entered the market in 1998, following extensive clinical trials by Serono. For 20 years Rebif© was manufactured at Interpharm’s plant in Israel (in 2005, production was moved to Switzerland). Revel and Rubinstein, both of whom served at various times as chief scientist for Interpharm, feel the company made a serious contribution to the Israeli biotechnology industry. A number of Weizmann Institute alumni made careers at Interpharm, and many have now been hired by the largest Israeli drug firm, Teva. Today, interferon beta-based drugs for MS are a $4.6 billion industry, taken by three quarters of those who are treated for the disease (Rebif© alone sold $1.45 billion in 2006).
Meanwhile, Revel’s group continued to explore new applications for interferon beta. In 1995, they discovered that a topical application of interferon in genital herpes is effective in preventing the recurrence of symptoms, and they are continuing to research this use. In addition, interferon beta turned out to be very effective in treating hepatitis C in some Asian populations, and Serono has recently completed clinical trials with Rebif© for this use.
In 2005, Rubinstein and Novick were awarded the Milstein Award from the International Society for Interferon and Cytokine Research, and Revel was named an honorary member of this Society. Revel also received the Israel Prize in 1999 and the 2004 Emet Prize for his contributions to interferon research and biotechnology. Fifty years since its discovery, Rubinstein and Novick are still making surprising new discoveries about interferon: A recent paper coauthored by Vlaimir Hurgin, Daniela Novick, Ariel Werman and Rubinstein and in collaboration with Charles Dinarello from the University of Colorado showed that interferon gamma often requires a second molecule to exert its antiviral and major immunoregulatory actions. Revel’s group, meanwhile, in addition to pursuing further medical applications for interferon beta, has gone back to one of the two original genes they discovered in 1980, named interleukin-6. Now, Revel and his team believe they can find important medical applications for interleukin-6, possibly in combination with embryonic stem cell technology, to repair the myelin sheaths around nerves, which are disrupted in many neurological diseases.