Hiding deep inside the bone marrow are special cells. They wait patiently for the hour of need, at which point these blood-forming stem cells can proliferate and differentiate into billions of mature blood immune cells to help the body cope with infection, for example, or extra red blood cells for low oxygen levels at high altitudes. Even in emergencies, however, the body keeps to a long-term plan: It maintains a reserve of undifferentiated stem cells for future needs and crises. A research team headed by
Prof. Tsvee Lapidot of the Institute’s immunology Department recently discovered a new type of bodyguard that protects stem cells from over-differentiation. In
a paper that appeared in
Nature Immunology, they revealed how this rare, previously unknown sub-group of activated immune cells keeps the stem cells in the bone marrow “forever young.”
Blood-forming stem cells live in comfort in the bone marrow, surrounded by an entourage of support cells that cater to their needs and direct their development – the mesenchymal cells. But the research team, which included postdoctoral fellow Dr. Aya Ludin,
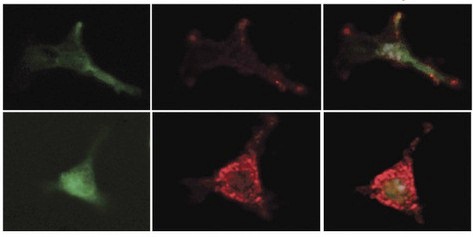
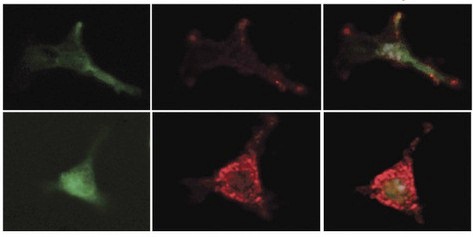
Prof. Steffen Jung of the Immunology Department and his group, and Ziv Porat of the Biological Services Unit, discovered another type of support cell for the stem cells. These are an offshoot of the macrophage family – literally the “big eaters” of the immune system that are important, for instance, for bacterial clearance. The team found that a rare sub-population of the bone-marrow macrophages has another role to play. Each of these rare macrophages can take a stem cell under its wing and prevent its differentiation.
Probing more deeply, the researchers revealed, in precise detail, how these macrophages guard the stem cells. They secrete substances called prostaglandins, which are absorbed by the stem cells. In a chain of biochemical events, these substances delay differentiation and preserve the youthful state of the stem cells. In addition, the prostaglandins work on the neighboring mesenchymal cells, activating the secretion of a delaying substance in them and increasing the production of receptors for this substance on the stem cells, themselves. This activity, says Lapidot, may help the non-dividing stem cells survive chemotherapy – a known phenomenon. Macrophages also live through the treatment, and they respond by increasing their prostaglandin output, thus heightening their vigilance in protecting the stem cells.
The bodyguard macrophages also increase their activity in times of infection. While other members of the macrophage family are recruited to fight the pathogens, their cousins in the bone marrow are hard at work ensuring that a pool of stem cells will resist the urge to differentiate.
In previous work in Lapidot’s lab, it was discovered that prostaglandin treatments can improve the number and quality of stem cells. This insight is currently being tested by doctors in clinical transplantation trials for the use of stem cells from umbilical cord blood to treat adult leukemia patients. These trials are showing that prior treatment with prostaglandins improves migration and repopulation potential, enabling the small quantities of cord blood stem cells to better cure the patients. “The present study hints at the possibility of further increasing the support for bone marrow stem cells by exploring this intriguing connection between the immune cells and stem cells,” says Lapidot. “An understanding of the mechanisms at work in these cells might improve the success of stem cell transplantation, especially that of umbilical blood.”
Prof. Steffen Jung’s research is supported by the Leir Charitable Foundations; the Leona M. and Harry B. Helmsley Charitable Trust; the estate of Olga Klein – Astrachan; the estate of Lola Asseof; Lord David Alliance, CBE; and the Adelis Foundation.
Prof. Tsvee Lapidot’s research is supported by the Leona M. and Harry B. Helmsley Charitable Trust. Prof. Lapidot is the incumbent of the Edith Arnoff Stein Professorial Chair in Stem Cell Research.