“Build your enemy a golden bridge to retreat across” is a piece of advice offered by Sun Tzu in his ancient military treatise, The Art of War. It turns out that cancerous growths adopt this strategy in their battle against the immune system. In a new study being published in Cell Reports, researchers from Prof. Idit Shachar’s laboratory at the Weizmann Institute of Science have discovered that a certain type of aggressive breast cancer prompts nearby immune cells to build “molecular bridges” between themselves, which causes these cells to refrain from attacking the cancer and leads to immune suppression. An antibody treatment that blocks the building of these bridges was shown to restore the immune system’s ability to attack with force, inhibiting the cancer’s progression in a mouse model.

In the past, cancer treatment focused on destroying the malignant cells by, for example, using radiation treatment or chemotherapy. In recent decades, however, it has become evident that a tumor’s development depends on the communication between the cancer and the nearby noncancerous cells. In an earlier study, researchers from Shachar’s lab in Weizmann’s Systems Immunology Department showed that blood cancer cells create “molecular bridges” with nearby support cells in order to survive and proliferate – otherwise they die within a matter of days. The researchers identified a protein, CD84 (SLAMF5), that is used to construct these bridges: When this protein is present on the surface of a specific immune cell, it can bind to a similar protein on a different cell, creating an intercellular bridge. In the type of blood cancer studied, CD84 is expressed in high quantities on the cancerous cells themselves, creating physical bridges between these cells and adjacent ones. The researchers even developed an antibody that blocks the bridges, slowing down the disease. As a result of these findings, the scientists began collaborating with the City of Hope cancer treatment and research center in California.
""We are presenting a treatment that might help a wide range of patients, since it focuses on the tumor microenvironment and not on the cancer cells themselves"
“We then wanted to see whether the molecular bridges between cells in the tumor’s microenvironment are also important in types of cancer other than blood malignancy,” Shachar says. “Dr. Steven Rosen, an executive vice president at City of Hope, proposed that we examine samples from patients with the most aggressive type of breast tumors – triple-negative breast cancer. One of the reasons there is still no cure for these tumors is that their cells show no external signs that would allow us to identify and destroy them. That’s why it is especially important to find a treatment that can suppress the cancer by affecting a component of its supportive microenvironment, rather than the cancer cells themselves.”
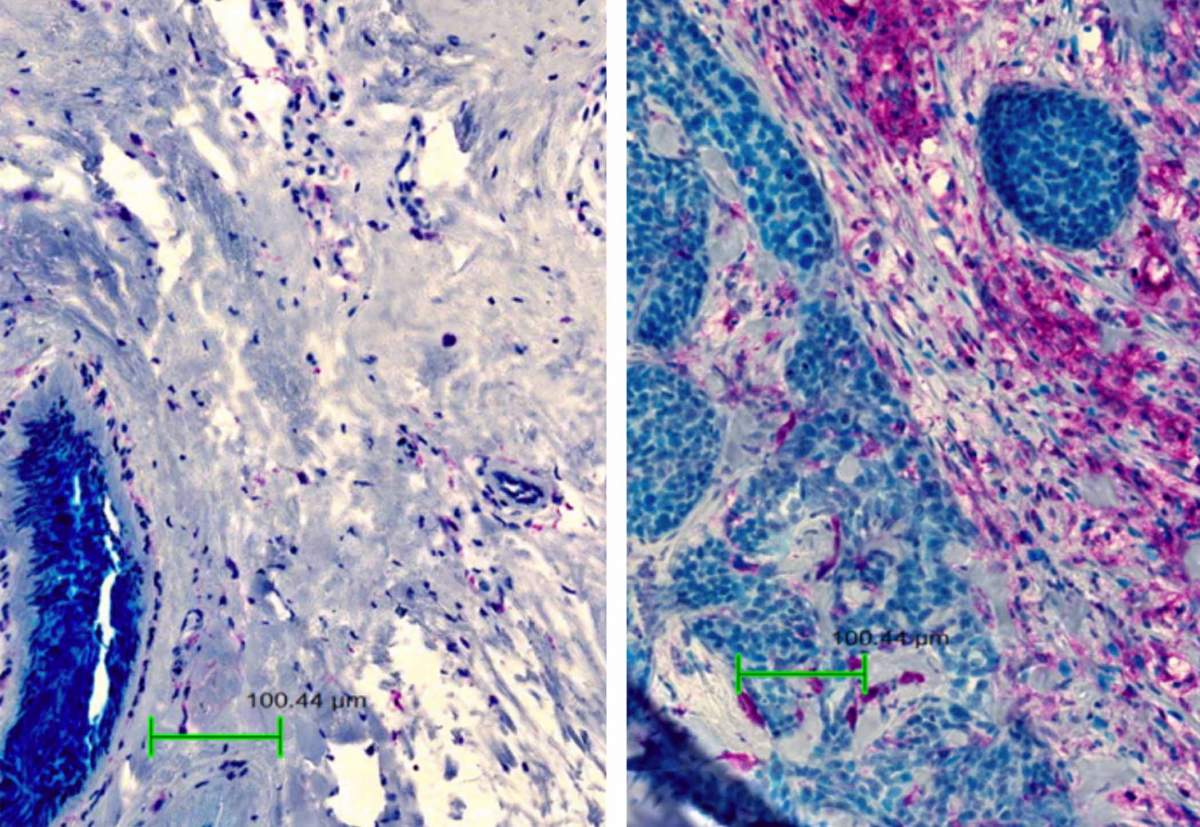
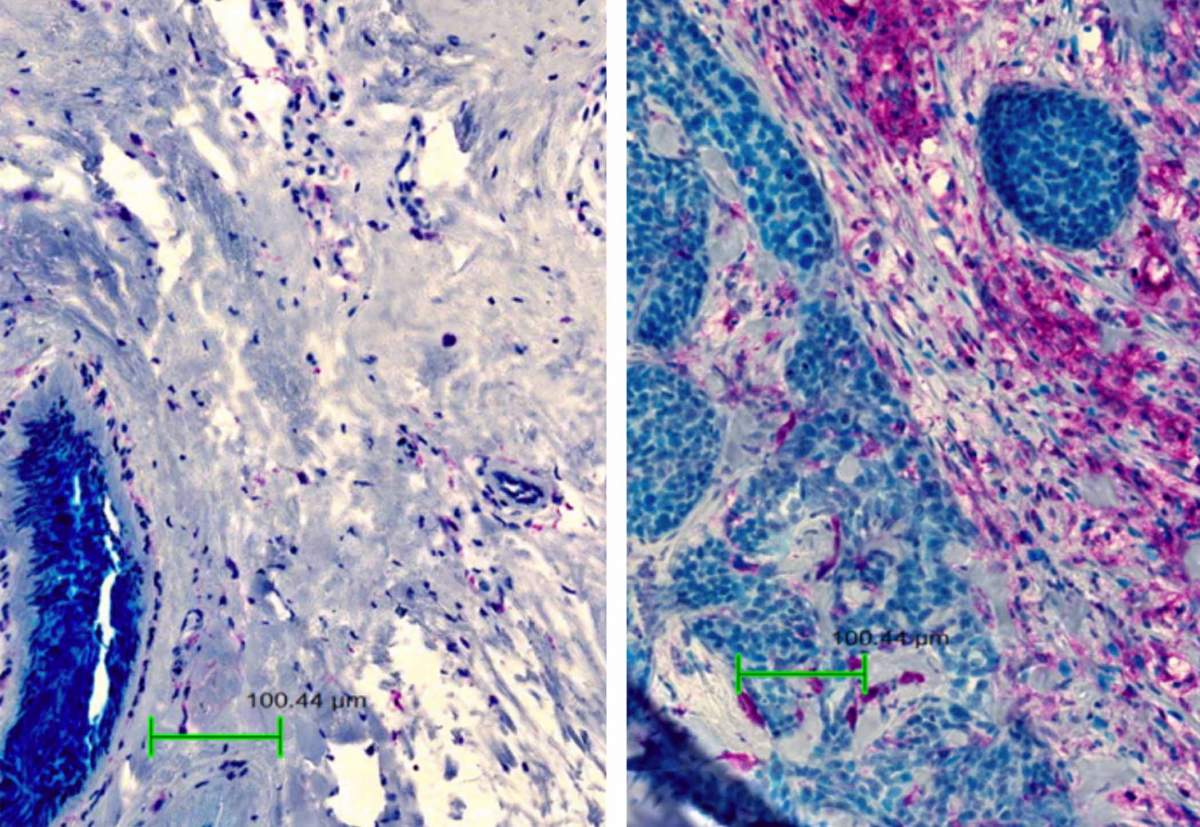
In the new study, led by Stav Rabani, a doctoral student in Shachar’s lab, the researchers analyzed the genetic sequences of growths taken from women with triple-negative breast cancer and discovered that the level of CD84 expression in the tumor microenvironment was much higher than normal. One of the surprising findings of the study was that even though breast cancer cells themselves express very low levels of CD84, they cause nearby immune cells to express it in large quantities and to create bridges between themselves, suppressing the immune response. The researchers also found that patients with higher levels of CD84 in their tumors did not survive as long as others.
Next, the researchers studied the progression of breast cancer in mice that had been genetically engineered not to express the CD84 protein and found that these mice developed significantly smaller growths. This finding prompted the scientists to test their previously developed antibody – which had successfully prevented the building of molecular bridges – as a treatment for breast cancer. Injections given twice a week to mice that had started developing breast cancer significantly slowed tumor growth and, in some cases, even led to complete recovery.
The researchers discovered that CD84 helps the cancer to develop by causing a buildup of cells that suppresses the immune response. They decided to focus on one of the cells that plays an unclear role in cancer – the regulatory B cell. They found that, like other immune cells, B cells build more “molecular bridges” in a breast tumor environment than in healthy tissue. The construction of the bridges causes these cells to produce a small protein that is known as a key suppressor of the immune response. When this protein is expressed in the tumor microenvironment, it is picked up by the immune system’s T cells – the warrior cells that are supposed to destroy the cancer cells – suppressing their activity and preventing them from attacking the tumor.
The City of Hope cancer treatment and research center, together with Yeda Research and Development Co Ltd, the commercial arm of the Weizmann Institute of Science, set up a company called Slam BioTherapeutics, which is developing cancer treatments based on anti-SLAM family antibodies. “The antibody we developed only works on cells that express a high level of CD84,” Shachar explains. “In a healthy person, most of the cells do not express this protein at all and immune cells express it at low levels, so the treatment works specifically in the tumor microenvironment. The company is currently focusing on using anti-SLAM antibodies to treat blood cancers in which the cancer cells themselves express high levels of CD84, but our new findings open the door to trying the antibody on many other kinds of growth, including those in which the cancerous cells don’t express this protein at a high level. In the age of personalized medicine, we are presenting a treatment that could help a wide range of patients since it focuses on the tumor microenvironment and not on the cancer cells themselves.”