Are you a journalist? Please sign up here for our press releases
Subscribe to our monthly newsletter:
Only the strongest survive. This is not always a good thing: Some very small, but very strong and very deadly survivors – cancer cells – may persevere after chemotherapy. In research that recently appeared in the Journal of the National Cancer Institute, Prof. Menachem Rubinstein of the Weizmann Institute’s Molecular Genetics Department suggests that cancer cells that have developed resistance to chemotherapy may have an Achilles’ heel that can be exploited to weaken them so they can be killed.
Following chemotherapy – a combination of drugs that kills tumor cells – the cancer sometimes comes back; and it may be stronger and more resistant to treatment than before. The pharmaceutical industry was focused for quite a while on proteins on the cells’ outer wall that act as “pumps” for expelling the drugs from the cell. But blocking these pumps did not solve the problem of drug resistance.
Rubinstein and his research group decided to take a step back and have another look at what makes a cancer cell resistant to chemotherapy. “We figured that if blocking the pumps did not solve the problem, there must be some other mechanism of resistance,” he says. The research conducted in his lab – led by visiting scientist Prof. Chiara Riganti from the University of Torino, together with Sara Barak – showed that a protein called CEBP can appear in cancer cells in two different forms. These two forms, called LIP and LAP, have opposite effects on the cancer cell.
Cancer cells that have developed resistance to chemotherapy may have an Achilles’ heel that can be exploited to weaken them so they can be killed
LAP, the long form of the protein, is a functional protein, while LIP, the short version, binds in the same way but does not perform any work. Earlier research in Rubinstein’s group had shown that LAP works to avert cell death when the cancer cells are exposed to stress, while LIP, because it binds to the same locations as LAP but does not carry through, actually expedites cancer cell death.
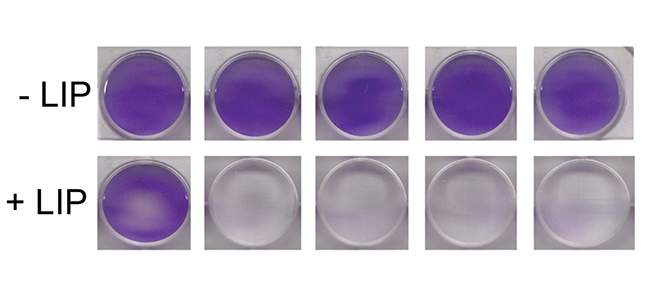
In the present study, Rubinstein and Riganti discovered, to their surprise, that chemotherapy-resistant cells from many kinds of cancer do not contain any LIP at all. When they inserted the genes for LIP into these cells, the cells began to respond well to the chemotherapy drugs.
Once again Rubinstein took a step back to ask: Why is there no LIP in these chemotherapy-resistant cells? Further investigation revealed that these cells actually do produce the short, LIP, form of the protein. It is just that the cellular degradation machinery takes LIP apart as soon as it is produced. The solution to the problem appeared to be simple: The scientists demonstrated that existing drugs that have been approved for other uses inhibited the process by which LIP is degraded.
Experiments with tumor cells cultured in the lab have yielded positive results. Much more research is required before we will know if the drugs are effective against cancers in the human body, but the scientists envision them being used in combination with current chemotherapy, weakening the cells’ resistance so that the chemotherapy can eliminate them.
Prof. Menachem Rubinstein’s research is supported by the Jeanne and Joseph Nissim Foundation for Life Sciences Research; the Bernard and Audrey Jaffe Foundation; and the Adelis Foundation. Prof. Rubinstein is the incumbent of the Maurice and Edna Weiss Professorial Chair of Cytokines Research.