"You don't assign him murder cases. You just turn him loose," claimed promos for Dirty Harry, a popular film of the 1970s starring Clint Eastwood. This daredevil cop-hero may now have a cellular counterpart fighting disease - a special type of cell that helps counter transplant rejection. When about to be attacked by another cell, this cell "draws" first and promptly destroys the attacker. Scientists refer to this cellular feat as "veto" activity because the cell has veto power over its own destruction.
Weizmann Institute researchers suggest that veto cells may have the ability to improve bone marrow transplantation, now performed mainly in leukemia patients, and make such treatment worthwhile for patients with non-lethal blood disorders. (In a bone marrow transplantation, stem cells from the donor's bone marrow are transplanted into that of the patient.) In the future, veto cells may also facilitate the transplantation of such organs as the heart, liver, and kidneys.
Until recently, doctors believed that for stem cell transplantations to succeed, a full match between the donor and recipient was necessary. Patients having no donor among their siblings must search the general population, but for roughly half of them a donor is found too late or not at all.
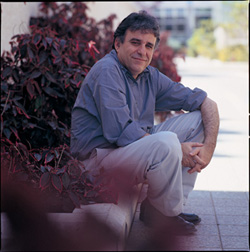
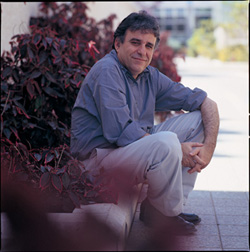
Over the past decade, Prof. Yair Reisner of the Weizmann Institute's Immunology Department, together with Prof. Massimo Martelli of Italy's Perugia University, has conducted research that has enabled transplants of partially matched stem cells in leukemia patients. Using this method, donor and recipient need be matched for only three of six immunological markers. Such a match is always present between parents and children, and there is a 75% chance of finding it among siblings. If the search includes the extended family, more than 95% of patients can find a donor.
Hundreds of patients throughout Europe have been treated using this approach, yielding significant success rates, according to the New England Journal of Medicine and other publications. These results indicate that mismatched transplants can be as effective as those in which donor and recipient are fully matched. Phase 1 studies are currently under way in major centers in the United States, and the European Bone Marrow Transplantation Society has recently launched a prospective study in more than 30 medical centers throughout Europe.
A key element of Reisner's approach is the use of extremely large doses of donor marrow, which literally overwhelm the recipient's rejection mechanism. The donor is treated with hormone injections that release a large number of stem cells from the bone marrow into the bloodstream, from where they are selectively removed. But how does bombarding the patient with a megadose of donor stem cells prevent transplant rejection? "Strength in numbers sounds simple enough," says Reisner. "Yet what are the underlying mechanisms?"
In two new studies, Reisner and his team members - Dr. Esti Bachar-Lustig, Rita Krauthgamer, Judith Gan, and doctoral students Shlomit Reich-Zeliger and Hilit Gur - provided insights into this riddle. They showed that the key to success lies in stem cells endowed with potent veto activity, which are capable of protecting themselves against rejection by the body's immune system. When these cells sense that they are about to be attacked, they impose their veto by selectively killing off the attacking immune cells without harming the rest of the patient's immune system. The success of megadoses would thus result from veto cells being present in larger numbers.
It may be possible to harness this veto mechanism to make bone marrow transplantation less demanding on the body. Currently, to reduce the risk of transplant rejection, the patient's immune system is suppressed using large doses of drugs and radiation that in themselves can be lethal. Reisner has shown that the number of veto cells can be increased 80-fold, and he proposes using larger numbers of such cells in a transplant. This approach should allow doctors to use lower drug radiation levels prior to transplantation, which in turn should reduce the side effects and the risk of mortality associated with the procedure.
While bone marrow transplantation is still considered too risky for patients with non-lethal diseases such as thalassemia and sickle-cell anemia, Reisner's gentler transplantation procedure may be appropriate for these diseases. The veto mechanism could improve the success rate of organ transplants as well: Veto stem cells could be injected at the time of the transplant to serve as "bodyguards" that prevent rejection of the transplanted organ.
Prof. Reisner's research is supported by the Gabrielle Rich Leukemia Research Foundation, Switzerland; the M.D. Moross Institute for Cancer Research; the UBS Optimus Foundation, Switzerland; Mrs. Erica Drake, New York; the Ligue Nationale Francaise Contre Le Cancer, France; Mrs. Renee Companez, Australia; and Stanley A. Lewis, New York, NY. He holds the Henry H. Drake Professorial Chair in Immunology.