Are you a journalist? Please sign up here for our press releases
Subscribe to our monthly newsletter:

Our immune system not only fights pathogens when they first make us sick – it continuously prepares for future attacks. Defenders such as antibodies are honed by competition to become better and better at destroying the pathogen. New research at the Weizmann Institute of Science shows that the immune system boosts its response capabilities with “amplifier” molecules that permit a varied selection of antibody-forming cells to enter special “training camps” for generating highly efficient antibodies. This strategy, according to study leader Dr. Ziv Shulman of the Immunology Department, gives the body broad protection against diverse strains of the pathogen.
Antibodies are proteins produced by white blood cells called B cells. Each B cell expresses a unique antibody on its surface, so some will excel in identifying each invader. Once a B cell has detected a pathogen, it starts to divide rapidly and differentiate. These cells secrete massive amounts of antibodies (1000 per second), spreading them through the bloodstream to destroy the pathogens. Most of these initial antibodies, however, can only bind weakly to the microbes they are fighting, and so they are a short-term defense.
“After the illness has passed and the pathogen has been cleared from the system, the body continues to refine its defense against it,” says Shulman. This refining, known as “antibody affinity maturation,” takes place inside the lymph nodes, in tiny “training camps” created for the purpose called germinal centers.
Inside the germinal centers, a sort of evolutionary process takes place in which the antibody-encoding genes undergo random mutation. The best mutated B cells are selected through a kind of competition, eventually becoming long-lived plasma cells that continue to provide protection for many years.
B cells must undergo a preliminary selection to enter the germinal center competition for affinity maturation. It was thought that only the cells with the highest starting affinity are selected to enter the training camps, but recent research has shown that the most protective antibodies against certain infectious agents, for example HIV and influenza viruses, actually start with very low affinity. These low-affinity antibodies appear to have the potential to become super neutralizers once they get into the training camps in germinal centers. “If the initial selection chooses the best pathogen-binders, how do the low-affinity antibodies get a chance to train?” asked Ziv. “To solve this problem, we needed to better understand how the selection process works for entry into the germinal centers.”
The judges for acceptance into both the affinity maturation process and those processes that take place later within the germinal centers are another type of immune cell known as helper T cells. The “selection” signals are delivered “personally.” These two cell types – T and B – must attach to one another physically for 30-60 minutes, during which they exchange messages through their outer membranes.
B cells bearing high-affinity antibodies present the T cells with the pieces of pathogen they have taken as “prizes” in their attacks. These gifts encourage the cells to prolong the contact and explore the possibility of admittance to the training camps. The question, says Ziv, was: “How can B cells whose antibodies display fewer pathogen prizes get the attention of the T cell selectors? We realized that there has to be an amplification mechanism at work. And since physical interactions are mandatory for this process, we looked for an amplifier of the cell-cell interaction or, in other words – an adhesion molecule.”
They examined the possibility that so-called Intercellular Adhesion Molecules, or ICAMs for short, could enable B cells to improve their communication with the T cells and thus intensify their signals. So they staged several experimental competitions, first with B cells engineered to lack ICAMs entered into the regular affinity maturation contests. While these lost out, further experiments showed that B cells with low-affinity antibodies plus ICAMs can outcompete high-affinity ones that lack them. In other words, ICAMs can compensate for reduced antibody affinity in the entrance competition. “But we still needed to answer the question of whether ICAMs do this by helping the cells stick together longer,” says Ziv.
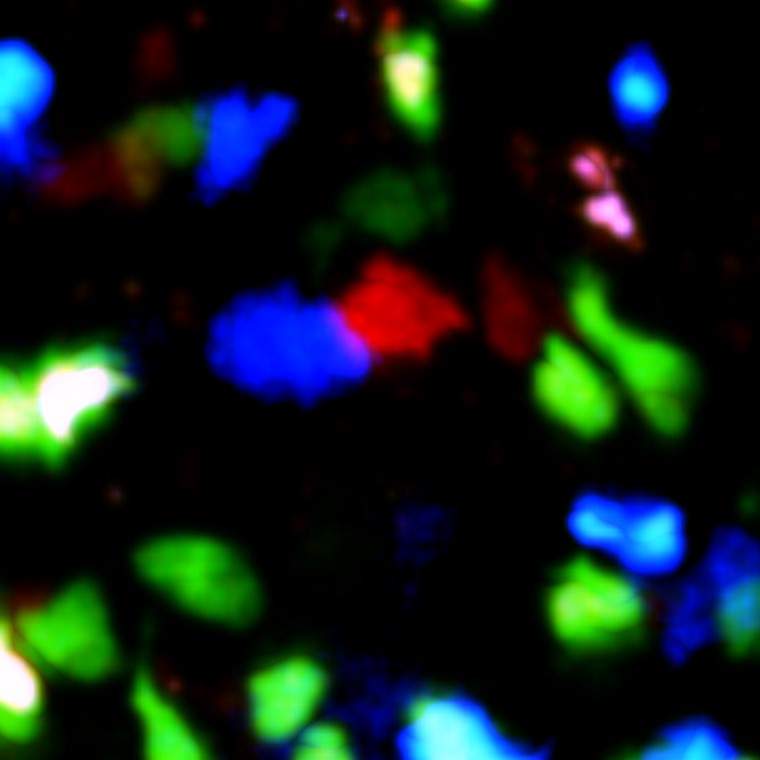
The team then used a special technique in Shulman’s lab that enabled them to observe, under a microscope, the dynamics of living cells in a mouse lymph node (in anaesthetized mice). The T and B cells were labeled in fluorescent dyes, enabling the researchers to closely follow the contacts between cells. They found that B cells with ICAMs were able to keep the contact with the helper T cells going for much longer than those without, giving them the opportunity to exchange multiple signals for extensive time periods and thus gain admittance to the germinal centers.
Today’s low-affinity B cells could be tomorrow’s high ones
Why should these lower-affinity cells be accepted into the immune program? “The low-affinity antibodies are wanted for their potential to change,” says Shulman. And since pathogens like HIV or influenza mutate rapidly, today’s low-affinity B cells could be tomorrow’s high ones. A wide diversity of antibodies provides broad protection, while a narrow group may be too specialized. ICAMs are what promote this diversity.”
These insights may aid in the search for better vaccines against such diseases as malaria, HIV or influenza, in which the pathogens vary from area to area, person to person, or season to season. In vaccination against these infectious agents, we might try, for example, to target the B cells with the most potential to mutate and form broadly neutralizing antibodies rather than the best initial variants. They could also help in the development of antibodies to be used as drugs, and they may have implications for research into the immune response to cancer.
Dr. Ziv Shulman's research is supported by the Morris Kahn Institute for Human Immunology; the Benoziyo Endowment Fund for the Advancement of Science; the Sir Charles Clore Research Prize; the Rising Tide Foundation; the Azrieli Foundation; the Comisaroff Family Trust; the Irma and Jacques Ber-Lehmsdorf Foundation; the Gerald O. Mann Charitable Foundation; the David M. Polen Charitable Trust; and the estate of Leah Arbel.