“Our working assumption,” says Livneh, “has been that small differences in the efficiency of those DNA repair mechanisms can affect individuals’ tendencies to get cancer. The combination of two factors – exposure to carcinogens and a lowered ability to repair DNA damage – will elevate the risk of developing the disease.”
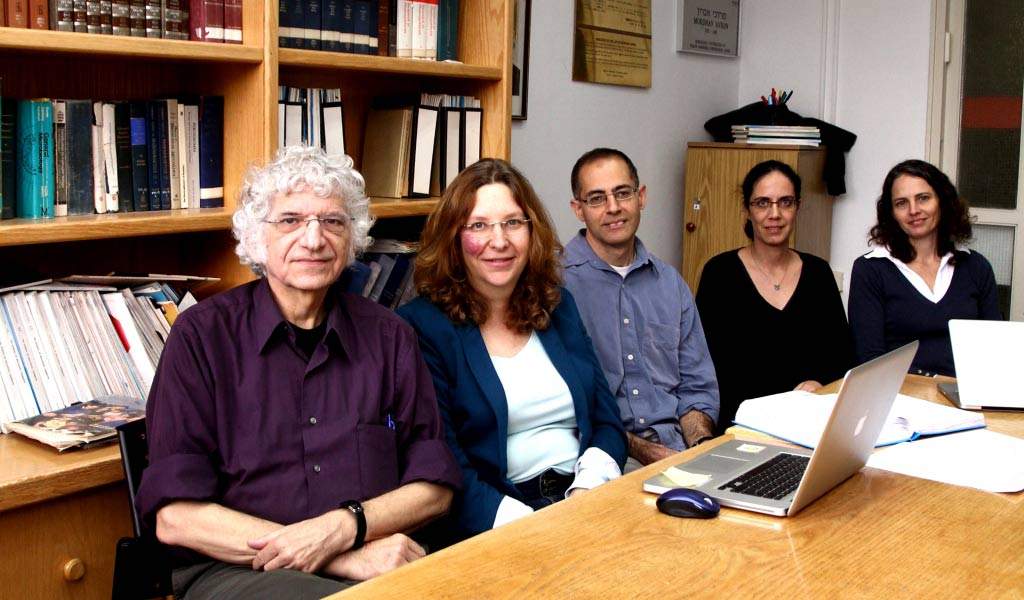
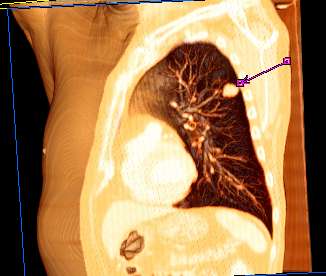
In the present study, Livneh, Paz-Elizur and Dr. Yael Leitner-Dagan set out to improve the accuracy of their predictions. They developed a method to measure the activities of a second repair machine, known as MPG. Like OGG1, MPG fixes oxidative damage, but unlike that enzyme, it deals with a broad range of injuries, among them those caused by chemotherapy. Together with Prof. Gad Rennert of the Technion and the Carmel Medical Center, and Dr. Ran Kramer of Rambam Medical Center, the scientists collected blood samples from 100 lung cancer patients and compared them, in a blinded test, with samples from 100 healthy people.
They found that there is, indeed, a correlation between MPG activity and the tendency to develop lung cancer, but this correlation was the opposite of what they expected: MPG was more active in the lung cancer patients. How could their results be explained? “There is a price to pay for the fact that MPG acts on a wide range of problems. It doesn’t always manage to cut out the injured bit,” says Livneh. “It can get ‘stuck’ to the DNA strand and block access for the repair machinery that is more specialized. So, high levels of this enzyme can be ‘too much of a good thing.’”
Using the activity levels of both enzymes to evaluate the lung cancer risk factor enabled them to better predict who would get the disease.
The findings were recently published in the
Journal of the National Cancer Institute.
The scientists hope their findings will not only result in a better test for lung cancer risk, but that they may aid in the development of ways to reduce the genetic sensitivity to carcinogen damage. For instance, a cocktail of drugs – one to raise OGG1 activity and another to lower that of MPG – could possibly restore the balance. Another avenue might be to find a common regulatory mechanism that controls the levels of both and adjust its function. Livneh and his team plan to check these possibilities using new equipment recently installed in the Israel National Center for Personalized Medicine at the Weizmann Institute.
Participating in the research were Dr. Ziv Sevilya and Dalia Elinger in Livneh’s group, and Mila Pinchev and Hedy Rennert in Rennert’s group. The statistical analyses were done by Prof. Laurence Freedman of the Gertner Institute for Epidemiology and Health Policy Research at Chaim Sheba Medical Center, and Prof. Edna Schechtman of Ben-Gurion University of the Negev.
Prof. Zvi Livneh's research is supported by the Y. Leon Benoziyo Institute for Molecular Medicine, which he heads; the Leona M. and Harry B. Helmsley Charitable Trust; Dana and Yossie Hollander, Israel; and the estate of Alice Schwarz-Gardos. Prof. Livneh is the incumbent of the Maxwell Ellis Professorial Chair of Biomedical Research.